Electromedical devices are medical devices used by healthcare industries for therapeutic use (surgical instruments, lasers and others) or diagnostic/monitoring use (imaging equipment, monitoring devices). Electromedical equipment finds application in various sectors, such as cardiovascular, ophthalmology, dentistry, physiotherapy, respiratory and orthopaedics.
The design of electromedical devices requires engineers to do more. Accuracy and reliability are crucial in this field, and designers and engineers have to follow strict rules and face several challenges to make electromedical devices design in the right way.
CHALLENGES IN THE ELECTROMEDICAL DEVICES DEVELOPMENT & DESIGN
1. Safety of electromedical devices
The first requirement that an electromedical device must meet is safety, both for the patient and for healthcare professionals. The IEC 60601 family of standards establishes the main requirements for electromedical equipment: safety, performance and electromagnetic compatibility. Conformity with these standards can only be achieved through a complete study of the product development cycle, starting with the selection of components.
In order to conform to regulations, it is necessary to ensure high galvanic isolation of circuits in equipment, using barriers or other protective solutions such as optocouplers or transformers. This is because electrical isolation is directly linked to safety. In addition, leakage currents must be minimized — or better, eliminated.
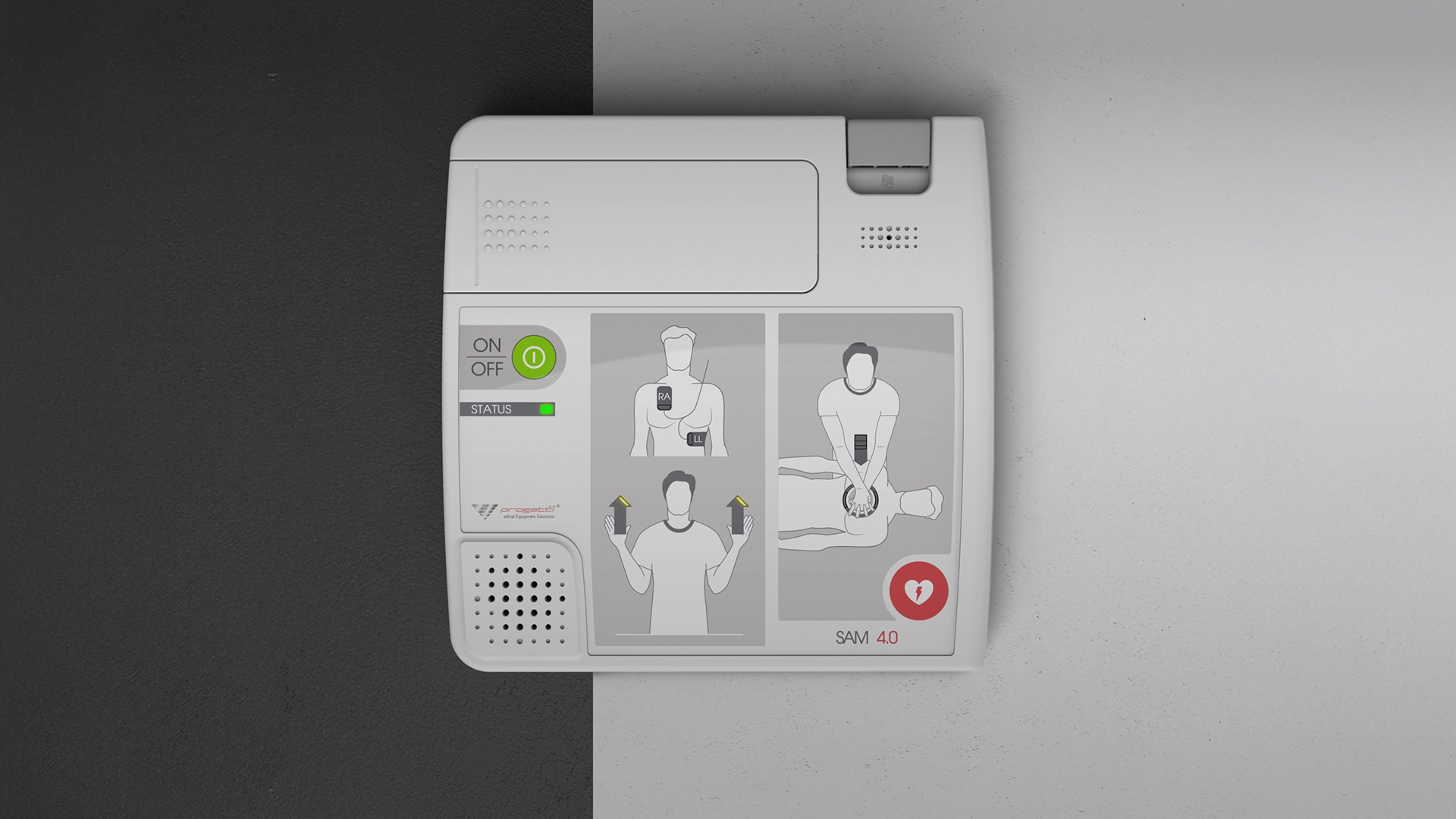
The highest risks exist for class III electromedical devices such as automated external defibrillators. Other electromedical devices, with lower risk classes (classes IIa, IIb and class I) are e.g. X-ray diagnostic equipment, lasers and ultrasound equipment.
2. Wearability of electromedical devices
The development of devices that monitor patients’ vital parameters or that programme and control the administration of drug doses has been made possible by the spread of the Internet and the IoT infrastructure. Such devices have made it possible to achieve significant savings on healthcare costs, and to improve the efficiency and quality of the treatments delivered. The success of these innovative systems lies in their connectivity and wearability.
A wearable electromedical device is an autonomous, non-invasive device capable of performing a specific medical function (such as monitoring or dosing drugs) for an extended period of time. The term wearable implies that the electromedical equipment must be directly supported by the human body or by clothing.
Wearable medical devices represent a major challenge for electronic designers.
The device’s battery must have a long service life, so power consumption must be kept to the bare minimum. To do this, the components must be chosen carefully, moving towards low-power solutions with the possibility of operating in sleep mode with low absorption. There are also important mechanical constraints related to size and weight that affect the electromedical devices design activity and favour the use of low-profile miniaturized components mounted on extremely compact PCBs.
Connectivity is also important for wearable electromedical devices: through a Bluetooth interface (typically BLE), a mobile network or WiFi, it is possible to connect to an application or gateway that can capture sensor measurements and control the operation of the device remotely.
3. Connectivity of electromedical devices
Connectivity concerns not only wearable devices, but also other types of electromedical equipment. The market for connected electromedical devices is growing, so there is a need to increase efficiency, reduce treatment costs and improve the treatment provided to patients.
Connected electromedical devices need to be able to connect to the healthcare system’s cloud infrastructure and to do so, they need a reliable antenna and network interface. A critical factor, often underestimated by companies that intend to place connected electromedical devices on the market, concerns the certification processes for wireless devices. In North America, for example, certification is separate from FDA tests and is required for all wireless devices.
Wheter a device is totally new, or is the upgrade of an existing device to which connectivity has been added, it needs to go through a rigorous certification process not only FCC and CE but (if using the cellular network) also with the mobile network operator.
4. Data Security
Regarding connectivity, another challenge is security. Connecting to the Internet will expose the data collected by the medical device to a potential breach. This is a serious issue in the medical device industry as it will lead to a breach of privacy and may prevent correct measurement and cause a subsequent incorrect analysis.
5. Components for medical applications
Every medical application has different requirements, but there is a common need: to use microcontrollers that can provide high performance in terms of processing times, reliability, safety, power consumption and connectivity.
The increase of connected devices is encouraging the introduction of computer security mechanisms that include the use of a chip. Furthermore, the demand for ultra-low power microcontrollers equipped with analogue peripherals is growing. The advantages of these devices are high reliability, low latency, low noise and lower costs. All very important features in devices such as glucose meters, heart rate monitors and implantable devices.
Another key component in the electromedical devices development is the DC-DC converter, whose special features are high isolation characteristics and low leakage current.
The main problem with thin, small and lightweight wearable devices will always be the operating time. Commonly used batteries such as lithium-ion (Li-ion) batteries, supercapacitor technologies or hybrid (combination of both) may be suitable for such devices.
TIPS FOR THE DESIGN AND DEVELOPMENT OF ELECTROMEDICAL DEVICES
The medical device must follow several regulations and pass safety tests. Often, designers and engineers have to modify a device that does not meet certain safety standards after it has been installed.
All device components must be certified or approved by regulatory agencies such as ISO and IEC. This is more expensive, but necessary.
In the electromedical devices design safety is very important and electrical insulation should be very accurate. What you need to do is to be aware of the amount of insulation required for your hardware from the beginning of the project, in order to revolve all production around this requirement and having to change the design later in the development process.
Like any other electronic equipment, electromedical devices can overheat. To make the device heat-resistant, first make sure that it is properly grounded. Next, choose an appropriate heat-sink. Also, make sure there is enough ventilation when designing. In the least likely scenario, it will be necessary to introduce a fan into the device.
Conformity with regulations and appropriate hardware components is crucial for the correct circuit design. With the creation of more powerful hardware, better processing units with safety protocols and wireless connectivity, the electromedical equipment is constantly changing to become safer and more reliable.
With many electromedical projects under its belt, Creanova can support you in electromedical devices design and electromedical devices development up to the contract manufacturing of your product. Whether your new device is a laser, a defibrillator or a wearable, our multi-disciplinary team has the skills and experience to guide your medical project throughout the development process and into contract manufacturing, ensuring high IP (ingress protection) level if required.
We can also help you with all the services you need for the electronics of your device: electronics engineering, PCB manufacturing and programming, SMT soldering and complete assembly (ISO 13485 certified) – electronics, mechanics and housings.
Contact us if you’re looking for a reliable partner to launch your electromedical device on the market!