Medical device prototyping is useful for testing the design and performance of a product beforehand. With prototyping, you can test materials and assess the potential market without a large investment of time and money.
Once you’re happy with your medical device prototype, you can move on to medical device manufacturing. To do this, there are several steps to take to make sure the transition to larger volumes goes smoothly. Here are seven tips to help you ease your new medical device development process and get the best results when it’s time to bring your product to market.
1. Define your schedule
Understanding how long the transition from prototyping to medical device manufacturing production takes is crucial to be able to assume a commercialization date.
The developer should use a checklist to verify that all requirements are met on time.
2. Create a Cross-Functional Team
The team should include representatives from engineering, manufacturing, materials management, quality, and business development departments. This variety of expertise will ease the transition from development to production.
3. Identify the suitable medical device Manufacturing Process
Plastic Medical Devices
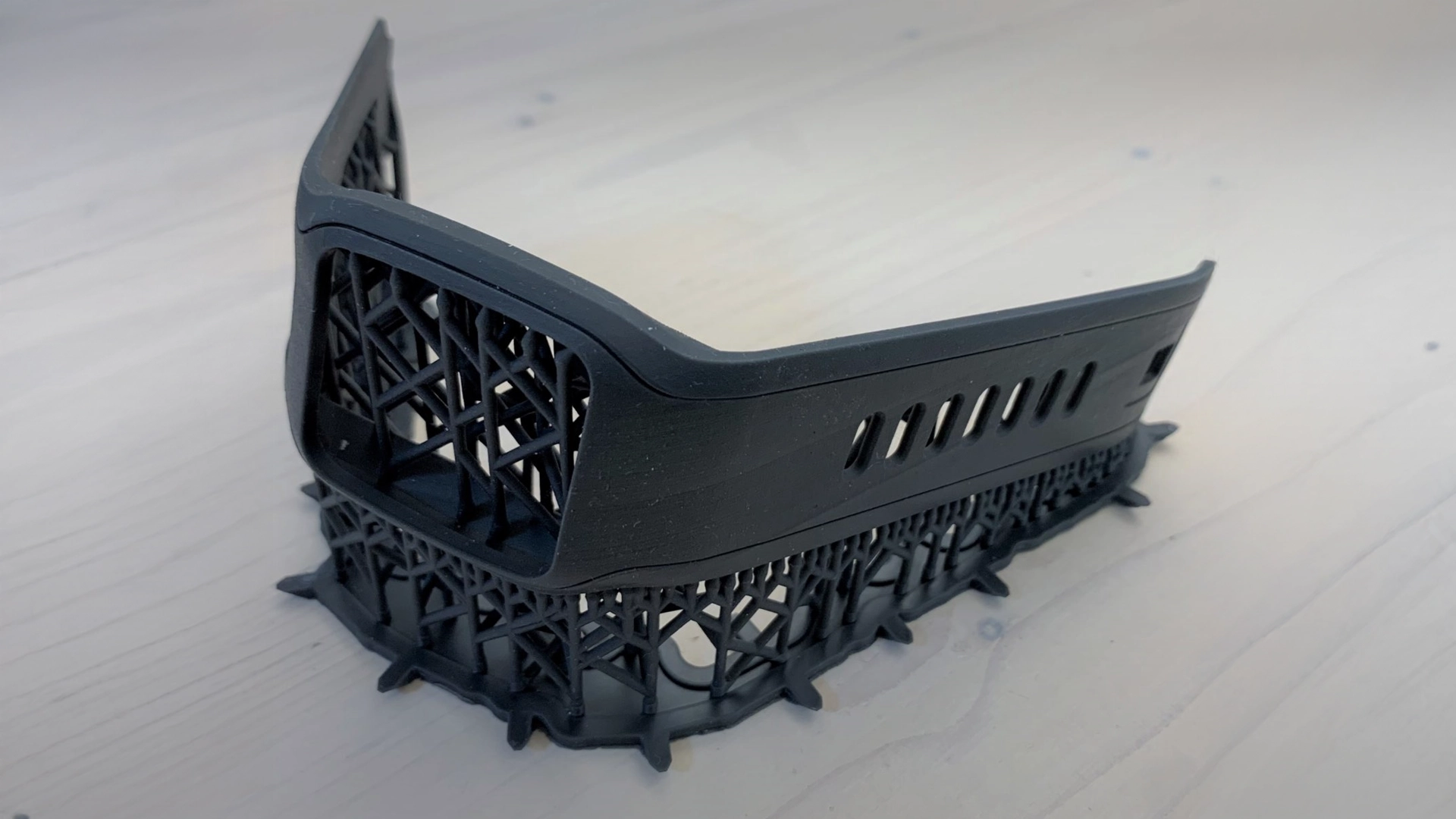
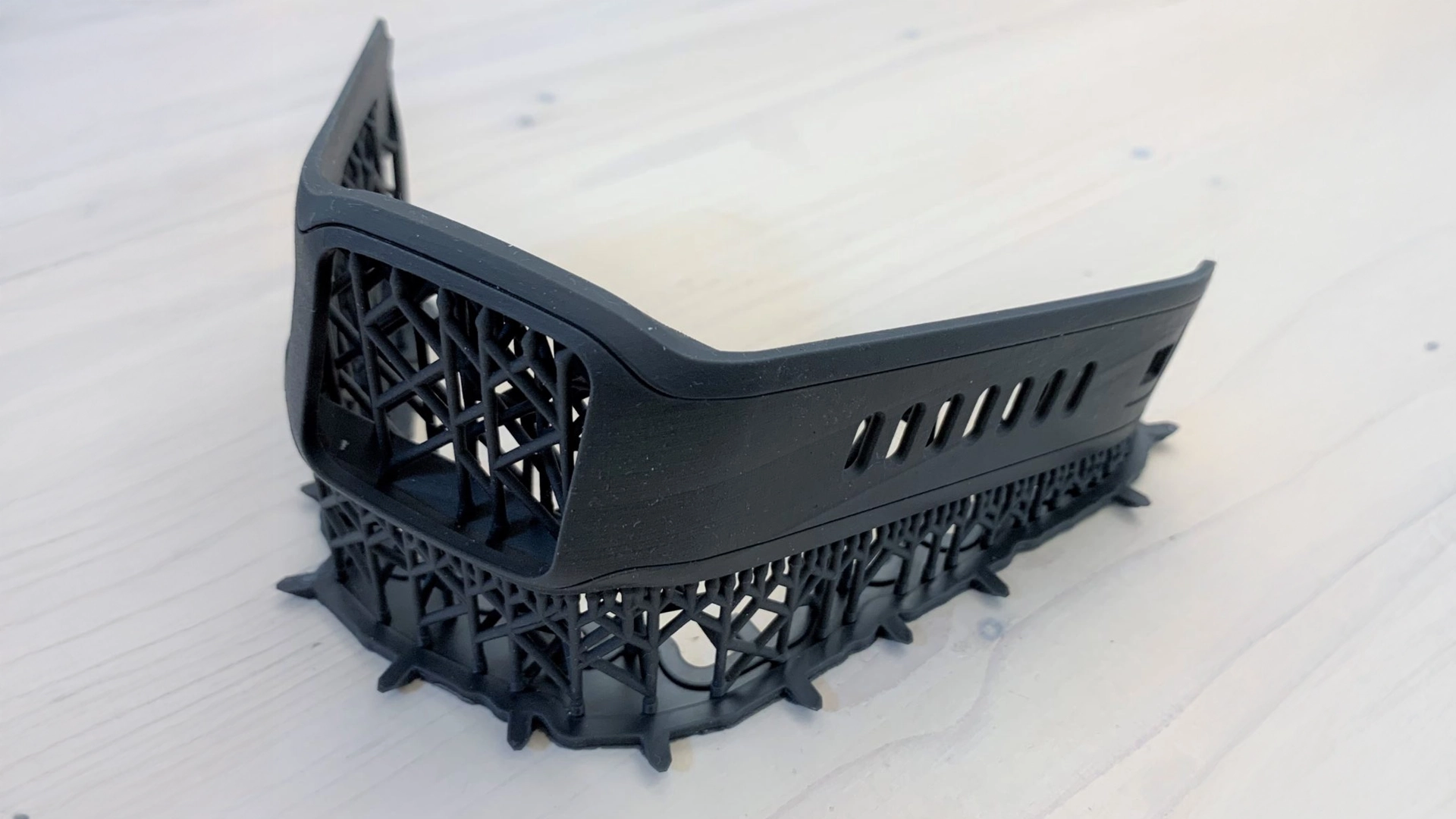
If the prototype is made of plastic, it is likely to be made by 3D printing, CNC machining or polyurethane vacuum casting. For larger quantities plastic injection molding for medical devices is the best solution.
Therefore, product developers must take into account the additional cost and time-to-market involved in transitioning from one process to another.
4. Create a BOM (Bill of Materials) and define production Setup Costs
Medical device prototypes usually have only a few fully finished parts and each one has a price tag.
This way at the time of production, every single element of the assembly can be accounted for. Every nut, bolt and screw, rubber button or metal clip, even the amount of paint or glue – everything has to be accounted for individually. Multiple line items indicate a more complex supply chain, so it pays to keep the design as simple as possible.
Finally, a detailed BOM can help you assess how much labor is involved in the assembly process, which can be a significant cost driver.
This will impose financial discipline as it will list all costs associated with a single production unit.
Knowing setup costs, such as those of molds and assembly equipment, will help you determine mass production cost.
5. Select The right Material
Sometimes the medical device prototype is made of an expensive or special material. The reasons for this are: to make it a showpiece, to help with a marketing or funding campaign and to meet some special technical requirements. But special materials are not a good choice for high volume medical device manufacturing.
Rather, using more common raw materials is indicated, investing more in finding a way around the problem that made that exotic material necessary in the first place. Common Raw materials are less expensive, easier and faster to source. Also, manufacturers are better able to work with this kind of materials, so it’s easier to get more reliable results. In addition, by using common raw materials, the choice of supplier will be more flexible and there will be less risk that the individual supplier will have problems with the supply chain, which could happen e.g. with the disruption of exotic material.
6. Conduct Final Testing & Verification
Once all parts have been manufactured, the medical device prototype or alpha/beta builds can be built, tested and verified to ensure they meet the customers’ desires. Testing is performed by both the internal and customer engineering teams to ensure they meet their quality and functional requirements.
This step allows the contract manufacturer to build a successful assembly plan to move into full-scale production. The information gained from building prototypes at the beginning will be used later for pilot and pre-production builds, or for full-scale production.
7. Plan for Certification
Unlike prototypes, parts suitable for commercial sale must be certified with safety and regulatory schemes such as CE and FDA approval. These will depend on factors including the environment the product is used in, whether it’s electrically powered, and the country where it’s sold.
Finished products will need to be sent to different organizations to obtain certifications, so the time and expense of this additional step needs to be calculated.
While this isn’t a complete list of the challenges you face, these steps just listed give a sense of the effort required to make medical device production transfer and hopefully provide you with enough knowledge on the topic.
When you want to launch your prototype as a commercial medical device, Creanova can help you out with a variety of manufacturing services to move from the medical device prototype to production.
As a Medical Device Contract Manufacturer, Creanova provides: medical injection molding, manufacturing (deep expertise in injection molding), PCB production and programming, Quality Control, Assembly (ISO 13485), Product traceability, Labelling & packaging, Warehousing & Logistics.
We also provide industrial design, engineering, prototyping and R&D support which make Creanova a full-service medical device product development company.
These are just a few of the reasons why medical device companies have been turning to Creanova to manufacture their medical devices for nearly 20 decades. Contact us to learn more.